Integral and Sustainable Air-conditioning in The Hospital Sector
For a proper comprehensive and sustainable air conditioning of hospitals, we must pay special attention to their physiological and hygienic requirements. Which means; we need to have a clear understanding of the desired environment within hospitals in general, and specifically within the various rooms found within these buildings.
To do this, we base ourselves on two regulations, these are the UNE 100713, recognised by RITE, and the UNE 171340, which complement each other and determine the internal conditions that each of the rooms in a hospital must have (ambient temperature, relative humidity and direction of air flows).

First of all, we must take into account the diversity of rooms and spaces in hospitals in terms of their needs and environmental requirements. For this reason, UNE 100713 classifies them into two types, depending on how demanding the room is in terms of air conditioning.
UNE 100713
-Premises class I: very high requirements
-Premises class II: usual requirements
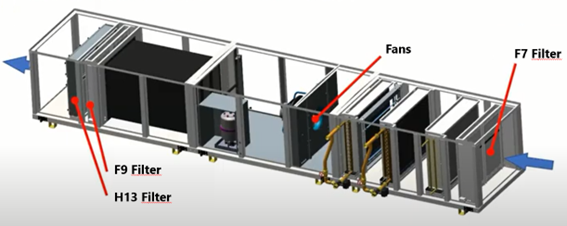
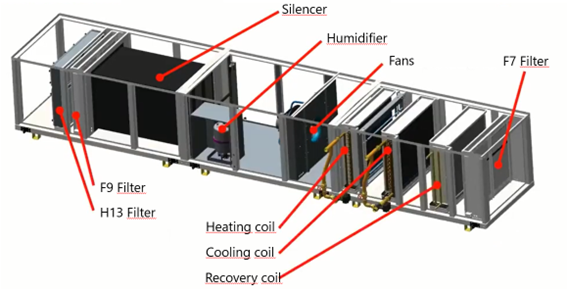
But what does it mean for a room to be Class I or Class II? Firstly, it determines what type of filtration it must have. Class 1, having much higher standards, has three levels of filtration, while class 2 has two levels of filtration.
| Filtration level | Filter class | Regulation |
|---|---|---|
| 1º | F 5 | UNE-EN 779 |
| 2º | F 9 | UNE-EN 779 |
| 3º | H 13 | UNE-EN 1822-1 |
In addition, the type of premises also implies the place where the filters have to be placed:
– 1st level: it is always placed at the outside air intake or at the air inlet of the air handling unit, as it cleans what may come from outside.
– 2nd level: at the beginning of the supply duct.
– 3rd Level: as close as possible to the room or premises so that the air enters the interior perfectly pure.
Another aspect to take into account when classifying rooms or spaces is the circulation of air between them. This is one of the basic problems that hospitals have, since contaminated air from some rooms or areas can pass to others where it should not be and can cause cross-contamination of infections, for example.
Based on this idea and the above classification, it should be clear that air circulation between rooms is only permissible when it is carried out from rooms with higher requirements, i.e. air from class I rooms, having higher requirements, can pass to class II rooms, but not vice versa.
On the other hand, when we talk about optimal air conditioning of hospital premises, we must talk about controlled environments or controlled environment rooms. These rooms are more complex, which require the level of risk associated with them to be defined in order to determine their technical specifications.
UNE 171.340 standard makes a division of 5 risk levels where 1 has the lowest requirements and 5 has the highest.
| Validation and qualification of controlled environment rooms in hospitals | |
|---|---|
| Risk 1 | Light |
| Risk 2 | Moderate |
| Risk 3 | Medium |
| Risk 4 | High |
| Risk 5 | Very high |
For example, an infectious corridor has a level 1 risk, while within the same sector, such as an operating theatre, we can find more than one level of risk; the operating theatre itself is level 4, while on the operating table (protected area) we find a level 5 risk.
Once the risk level associated with a particular room has been defined, among the default technical specifications we must mention the complete air renewals. Depending on the risk, the room will have more or less air renewal.
Another of the technical specifications included in UNE 171.340 is the classification of the rooms. We find ISO 5, ISO 6, ISO 7, ISO 8 or ISO 9 rooms. In addition, it also takes into account whether the installation is in operation or at rest. It also has to be taken into account whether the room should be overpressure or underpressure depending on whether it is in operation or not.
And of course, another specification that depends on the risk level is how clean the room environment should be. For example, in the three highest risk levels, if we are at rest we may have some mesophilic aerobes, but in terms of moulds and yeasts it determines the absence of these.
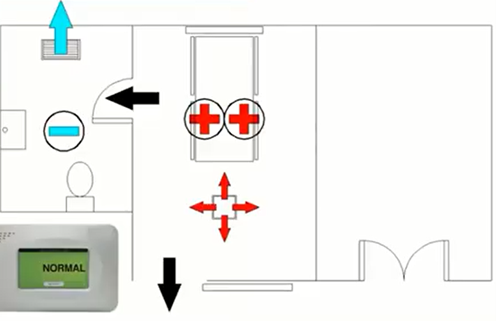
On the other hand, it is also important to talk about pressures, negative and positive. Negative pressure rooms are usually infectious or contagious rooms; this means that the air inside the room should not go outside the room. Whenever we have something that we want to confine, we must have negative pressures. For this we must air-condition by injecting the necessary rate of fresh air and always have a depression in an adjoining room, a bathroom for example, to make the air flow from a dirty area to an even dirtier one. It is necessary to provide air locks between rooms, which are a first barrier, to avoid soiling clean rooms.
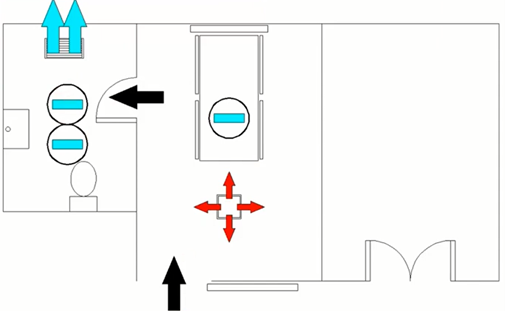
In the case of rooms where immuno-compromised people are found, for example, positive pressures are required, as the aim is to ensure that nothing dirty or infected enters the room and affects the patient. In order to achieve this, the purest possible air from the ATU must be injected.
Another of the most complex areas in hospitals are the laboratories, as they work with complex and different compounds such as formaldehyde or formaldehyde, among others, and therefore ventilation and extraction must be controlled. Normally, laboratories must be overpressurised and extractions are close to the door.
We have mentioned the existence of formaldehyde in laboratories, as before 2018 it was considered a substance that was probably carcinogenic, but since then it has been included in the list of substances that are carcinogenic to humans. This means that with the new regulations, formaldehyde sensors must be included in laboratories to monitor this compound.
When talking about hospitals, it is essential to mention the room that requires the most control, which is the operating theatres. First of all, we must take into account that within these there are two types A and B, with risk levels ranging between 3 and 5. Type A would be an operating theatre where a transplant is performed, while in type B a less complex intervention such as the removal of an appendix is performed.
In addition, as mentioned above, within the operating theatre itself there may be different levels of risk: level 5 in the stretcher or protected area and level 4 in the periphery.

There are tests such as the Segregation Test or the Recovery Test that are used to validate and check that the protected area has the optimum environmental conditions and correct ventilation of the space. For this, it is essential to have an AHU to ensure the necessary hygienic and physiological requirements.
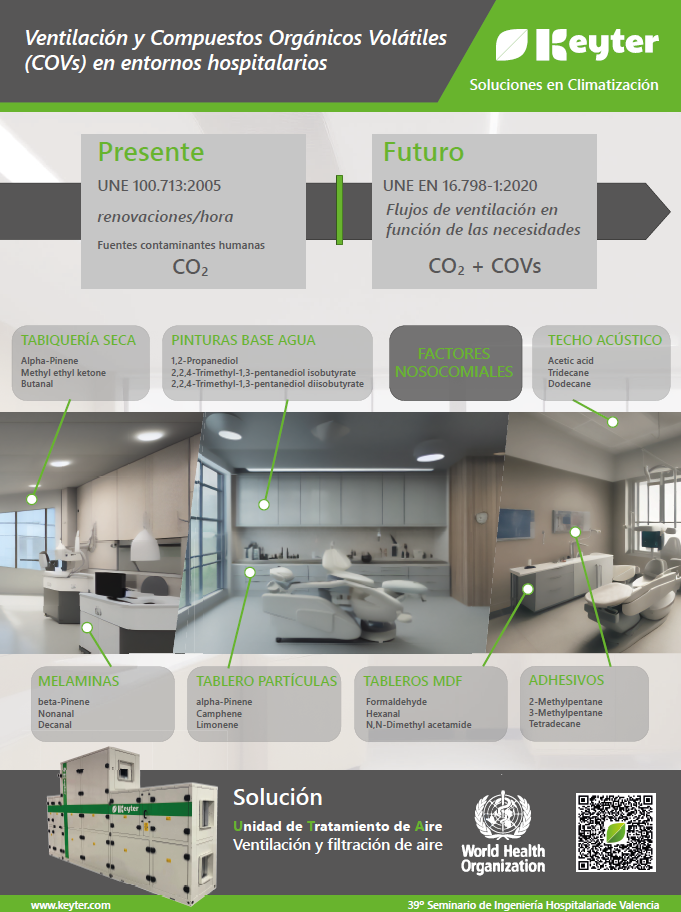
Finally, it is worth mentioning the new trends in ventilation and volatile compounds in Spain following the European framework, which are included in the UNE EN 16798 standard, which no longer speaks only of complicated places within a hospital, but also of a hospital in general and of the ventilation that we are going to use from now on in any type of building. You can learn more about these new trends in our article:
More articles
Interested in other (technical) knowledge articles? Keep yourself up to date and read them all