Hospital Air Conditioning
Jose Arboledas, Training and Special Project Responsible at KEYTER
The Regulations of Air Conditioning and Ventilation of Hospitals are wide, the diversity of Zones to be air-conditioned and ventilated so indicate. From corridors to operating rooms, from delivery rooms to examination rooms, … the typologies and needs are very varied and different. Until today, where one characteristic is common to all, the defense against SARS-CoV-2.
In a hospital environment they are no longer only governed by Regulations, Regulations or Directives, each Center goes beyond these provisions to improve its facilities based on its experiences and observations. The Standards indicate this since to classify a Controlled Environment Room a very high range of parameters must be taken into account.
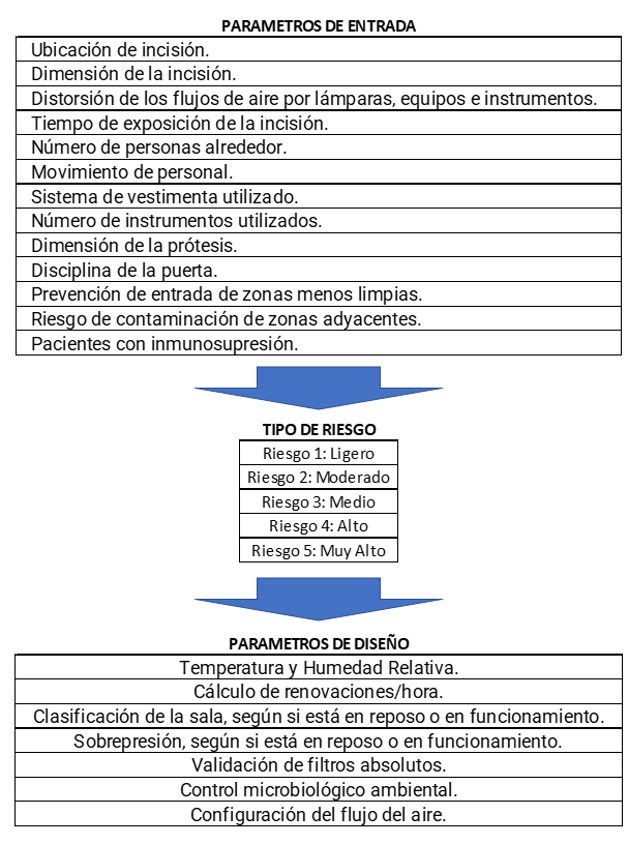
The following table (UNE 171340:2020) indicates the sequence of infection risk determination of a Controlled Environment Room.
HYGIENIC APPLICATIONS
Obviously, the most directly affected air conditioning installations are the operating rooms, and therefore those to which an even more special importance is granted, which must have controlled the temperature, humidity, contribution of outdoor air, quality and cleanliness of the air, overpressures …


In this case we have operating rooms of several categories, let’s see the most important characteristics of each of them:
Class A. High-tech operating rooms (ISO Classification 5 and 6)
Intended for:
Heart, lung, and liver transplants
Extracorporeal and aortic heart surgery
Orthopedic prosthesis surgery

The filtering of class A is carried out in 3 stages:
Pre-filter EU4
Climate control output filter EU9
Final filter in the operating room H‐14 o U-15 (For very exceptional cases)
Overpressures: +10 Pa
ISO Class 5 Classification
– Laminar flow in room
– In the operative field a recirculation flow of 80 movements / hour with a maximum air velocity at the diffuser outlet of 0.2 m/s
– Minimum contribution of outside air will be 1,200 m³/h, and the difference will be made with recirculated air, which will comply with the following parameters:
• The air will be from the operating room itself, only from this one, and therefore there will be a unique air treatment system
• The recirculated air will be treated the same as the outside air by the same air conditioner
• There must be microbiological control
ISO Class 6 Classification
– Turbulent flow in the room
– Recommended recirculation flow of 40 movements/hour
– Minimum contribution of outdoor air will be 1,200 m3/h will be outdoor air, which will comply with the following parameters:
• The air will be from the operating room itself, only from this one, and therefore there will be a unique air treatment system
• The air will be from the operating room itself, only from this one, and therefore there will be a unique air treatment system
• The recirculated air will be treated the same as the outside air by the same air conditioner.
• There must be microbiological control.
• The residual air velocity in the occupation zone or operative field defined above will be between 0.2 and 0.3m/s
Class B. ISO 7 Classification
Intended for:
- Conventional, emergency and major outpatient operating rooms
- Intended for the rest of surgical interventions.
The filtering of class B is carried out in 3 stages:
Pre-filter EU4
Climate control output filter EU9
Final filter in the operating room H‐13
Overpressures: +10 Pa
– Turbulent flow in the room
– Recommended recirculation flow will be at least 25 movements/hour
– Minimum contribution of outdoor air will be 1,200 m3/h will be outdoor air, which will comply with the following parameters:
- The air will be from the operating room itself and only from it, and therefore there will be a unique air treatment system
- The recirculated air will be treated the same as the outside air by the same air conditioner.
- There must be microbiological control
- The air velocity in the occupation zone, defined in these recommendations, will be 0.2 and 0.3 m/s.
Class C. ISO 8 Classification
Intended for:
- Ambulatory minor surgery operating rooms, delivery rooms and endoscopies
Class C filtering is done in 2 stages:
Pre-filter EU4
Climate control output filter EU9
Overpressures: +5 Pa
• Turbulent flow in the room
• Recommended recirculation flow will be at least 15 movements/hour
• Minimum contribution of outside air will be 1,200 m3/h
• The air velocity in the occupation zone, as defined in these recommendations, shall be 0.2 and 0.3 m/s.
As you can see, each of them is different and needs special characteristics that must be met, both the installation and the UTAs
COMMISSIONING
The work is not only in the design and installation of the equipment, the reception of the installation is a difficult task that must go through various phases to give the go-ahead to the whole.
All the component elements of the installation must be reviewed and their correct installation and operation verified.
Filters should be checked at three levels. The tightness of the filter material, the tightness of the frame and the tightness of the filter-frame joint should be checked
This supposes an absolute certainty that the air that is introduced into the room has passed through the filter, cancels the existence of by-passes.
This action must be carried out in each filter replacement, which indicates that the maintenance of this type of installation must be correctly studied and planned, in no case can it be treated as another installation.
The entire installation must be sanitized, in our case with hydrogen peroxide, so as to ensure the sterility of the system.
The air of the Critical Rooms must be analyzed as follows:
Particle counting: The counting of particles in premises with a high demand environment is carried out directly in the driven air. To do this, if necessary, a test aerosol is introduced in front of the last level of filtration, as an indicator, to detect possible leaks. For each air outlet, at least 3 checks are carried out.
Measurement of the concentration of microorganisms in the air: To carry out these measurements, at the discretion of the hygienist, suitable cultures are carried out with which the measurements can be made correctly.
Checking the direction of air flow: The verification of the direction of air flow must be carried out, with the room closed, by means of the smoke test. For the premises of the operating room area, this check, in addition to being carried out with the nominal flows, it is also necessary to carry it out with reduced air flows, outside the normal hours of operation.
UV-C and FILTRATIONS
Ultraviolet C (UV-C) light has been identified as one of the most important barriers to prevent aerial spreads of SARS-CoV-2. Its germicidal action has been shown to be effective, both on surfaces and in air, by deteriorating the RNA of the virus and preventing its replication within our cells. The water purification sector has been working with this type of device for a long time with very satisfactory and contrasted results. The list of pathogens that we can deactivate with UV-C is extensive, common diseases such as influenza could be alleviated, and its study has been long carried out and documented.
For this reason, the Hospital has been equipped with equipment for waiting areas and corridors, places of high traffic where contagion is very likely.
The two sanitization systems that combine the Air Treatment and Purification Units are the following:
HePA Filtration Sanitization – Particulate Matter (PM) in its three formats MP10, MP2.5 and MP1.0
Activated Carbon Filtration Sanitization for:
• Volatile organic compounds (VOCs)
• Ozone (O₃): Formed in the atmosphere by sunlight – NOx reactions
• Nitrogen dioxide (NO₂): Coming from organic combustion in the form of NO and main source of ozone when oxidized as NO₂.
• Sulfur dioxide (SO₂): Fossil fuels
ENERGY RECOVERIES
As has already been evident, the contagion is airborne for the most part, so special care was taken with the treatment of the airs of the Hospital.
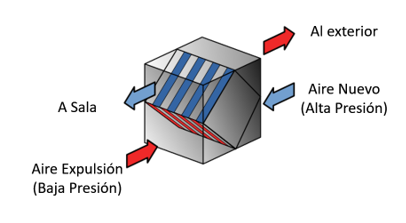
From the beginning of the pandemic, the need for heat recuperators not to bypass airs of expulsion into the new air circuit to avoid cross-contamination was indicated. Term of the field of food, where contaminated food contaminates fresh food, but in this case it is very parallel and graphic
This was the reason why the rotary recuperators stopped, which is highly advisable. In the case of cross-flows the probability of by-pass is minimal, but it exists. If the joints between walls ceased to be watertight we could find airs of expulsion, coming from the premises, which would pass to the new air ducts, supposedly clean, creating a risk of contagion when a recirculation is generated.
For this reason it was decided to overpress the new airs in front of the airs of expulsion. So, in the event of an air leak, it could not enter from the ejection circuits to the new air circuits, but the other way around, which does not entail any risk.
How do you achieve this?, simply by touching the slogans of the fans, a little more pressure and problem solved. Therefore, the Air Treatment Units (UTAs) that were supplied have this additional pressure in new airs.
ENERGY APPLICATIONS
The needs of air conditioning in a Hospital are very varied, although thermal control dominates, hygrometric control is also necessary. Operating rooms need constant Relative Humidity control, so in winter, apart from heating, it is necessary to dehumidify. This is where considerable energy savings are achieved, since the latent power of dehumidification is obtained free of charge from the heating power.
Although it may be contradictory, get cold from the production of heat, but Heat Pumps have this virtue, action – reaction, cooling power – heat power, having both sides of the coin.
Multipurpose equipment can work in this way, really in 3 ways:
• As a Cold Air-Water equipment
• As air-water equipment in Heat
• As a Water-Water in Cold and Heat equipment simultaneously
In this way, displacing the traditional boiler, we supply heat to the environment and by recovering the cooling power generated, it is dehumidified free of charge.
A single piece of equipment covers the functions of water chiller and boiler, with very high energy savings.

BIBLIOGRAPHY
– UNE 100713:2005 Air conditioning facilities in hospitals.
– UNE-EN ISO 14644-1:2016 and its 16 parts on Clean Rooms
– UNE 171340:2020 Validation and qualification of controlled environment rooms in hospitals
– NTP 859 (INSHT)
– ASHRAE – HVAC Desing Manual for Hospitals and Clinics. American Society of Heating, Refrigerating and Air-Conditioning Atlanta
More articles
Interested in other (technical) knowledge articles? Keep yourself up to date and read them all.